Introduction
Multiple myeloma (MM) bone disease remains one of the most devastating complications of this incurable cancer, causing bone fractures, pain, mobility issues and neurological deficits. MM cells produce osteoclast-activating factors that induce osteoclast activation, thereby leading to excessive bone resorption and lytic bone lesions1. Our previous work demonstrated that matrix metalloproteinase 13 (MMP-13) is a critical osteoclastogenic factor that is highly secreted by MM cells. MMP-13 induces osteoclast fusion and bone-resorption via a mechanism independent of its proteolytic activity2. We recently reported that MMP-13 binds to checkpoint inhibitor programmed death-1 homolog (PD-1H/VISTA), a surface receptor that is expressed in osteoclasts at high levels3. Binding of MMP-13 to PD-1H/VISTA induces osteoclast fusion and bone resorption activity whereas knockdown or knockout of PD-1H/VISTA largely block MMP-13 mediated effects on osteoclasts3. However, the function of PD-1H inMM bone disease in vitro or in vivo has not been previously defined.
Methods and Results
To confirm the role of PD-1H in MMP-13 induced bone disease in MM, we first conducted MM-osteoclast trans-well co-culture assay using murine MM cell line, 5TGM1 cells, and bone marrow mononuclear cells from Pd-1h-/- or wild type (WT) mice. 5TGM1 control cells or MMP-13 knockdown 5TGM1 cells were seeded in the upper wells of the transwell plates; while WT or Pd-1h-/- bone marrow mononuclear cells were seeded in the lower wells and cultured for osteoclast differentiation assessed by TRAP staining. Results show that 5TGM1 induced differentiation of WT osteoclasts with significantly increased osteoclast size and nuclei number/osteoclast. Consistent with our previous results2, MMP-13 knockdown blocked the 5TGM1 MM cells-induced activation of WT osteoclasts. In contrast, neither 5TGM1 MM cells nor MMP-13 knockdown cells had significant effects on Pd-1h-/- osteoclasts. Hence, knockout of Pd-1h abrogated MMP-13 mediated MM induction of osteoclasts, indicating that MMP-13/PD-1H interactions are critically involved in MM-induced osteoclast activation.
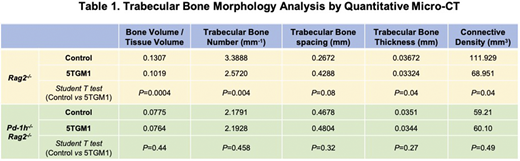
The in vivo role of PD-1H in MM bone disease was investigated using the intratibial 5TGM1 Rag2-/- MM bone disease mice model2. For this purpose, Pd-1h-/-Rag2-/- mice were generated by crossbreeding C57BL/6 Pd-1h-/- with C57BL/6 Rag2-/- mice. 3x105 firefly luciferase expressing 5TGM1 cells (5TGM1-luc) were intratibially injected into age and sex-paired Rag2-/- or Pd-1h-/-Rag2-/- mice (N=5). Tumor progression was monitored by weekly bioluminescence imaging (BLI). 3 weeks after tumor inoculation, tibiae were harvested for quantitative micro-CT, followed by histological analysis. Histological staining showed that intratibial injection of 5TGM1-luc MM cells induced extensive lytic lesions and trabecular bone loss in Rag2-/- mice. In contrast, in Pd-1h-/-Rag2-/- mice,the bone structure was maintained with markedly less bone loss. Morphological analyses of trabecular bone across proximal tibiae further indicated that in Rag2-/- mice, 5TGM1 induced significant changes in bone microarchitecture, with decreased bone volume fraction (bone volume/tissue volume), connective density, trabecular bone numbers, and trabecular bone thickness, as well as increased trabecular bone spacing (Table 1). In contrast, in Pd-1h-/-Rag2-/- mice, 5TGM1 failed to induce significant loss of trabecular bone, confirming the critical role of PD-1H in MM induced bone disease in vivo.
Conclusions
Taken together, our study, for the first time, reveal that checkpoint inhibitor PD-1H/VISTA is the critical receptor for MMP-13 in osteoclasts, thereby mediating MMP-13-induced osteoclast fusion, activation and bone resorption. MM-induced trabecular bone loss was significantly lower in Pd-1h-/-mice, demonstrating that PD-1H/VISTA plays a critical role in MMP-13-induced MM bone disease. Given the checkpoint role of PD-1H/VISTA in cancer immunosuppression, we further posit that targeting the interaction of MMP-13 and PD-1H may represent a novel therapeutic strategy to treat MM bone disease and modulate the MM immune environment.
References
1. Marino S, Petrusca DN, Roodman GD. Br J Pharmacol. 2019;10.1111/bph.14889.
2. Fu J, Li S, Feng R, et al. J Clin Invest. 2016;126(5):1759-1772.
3. Fu J, Li S, Yang C, et al. Blood. 2019; 134 (Supplement_1): 3072.
Lentzsch:Caelum Biosciences: Current equity holder in private company, Membership on an entity's Board of Directors or advisory committees; Janssen: Consultancy; Celularity: Consultancy, Other; Magenta: Current equity holder in private company; Karyopharm: Research Funding; Mesoblast: Divested equity in a private or publicly-traded company in the past 24 months.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal